- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Humanitarian Assistance
- Transformation at USAID
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab
Speeches Shim

At a Glance
- Introduction
- Scope of the Problem
- Components of Emergency Nutrition Response
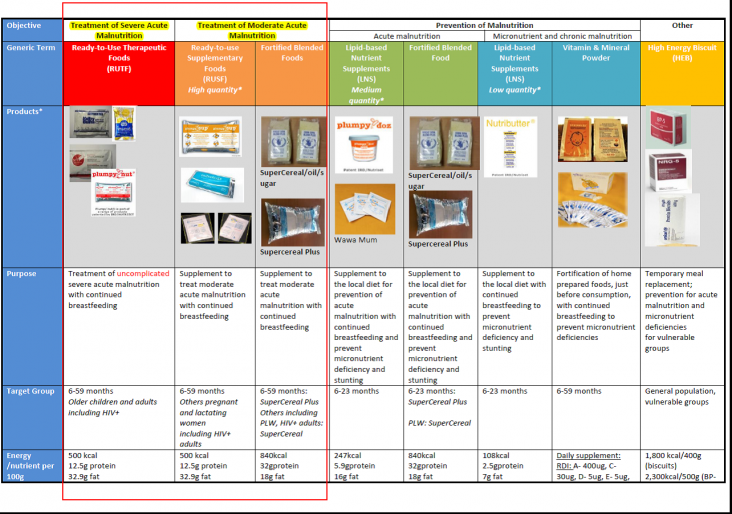
- Nutritional Products
- Examples from the Field
- Technical Resources
- References
- Endnotes
View the PDF [PDF, 1.0MB].
Introduction
Humanitarian crises exacerbate nutritional risks and often lead to an increase in acute malnutrition. Emergencies include both man-made (conflict) and natural disasters (floods, drought, cyclones, typhoons, earthquakes, volcanic eruptions, etc.). Complex emergencies are combinations of both man-made and natural disasters, often of a protracted nature. Millions of people are affected by humanitarian crises every year. In 2014 and 2015, a record number of large-scale humanitarian crises took place across the world: Central African Republic, Iraq, Philippines, Nepal, South Sudan, Syria, and West Africa (Ebola).1 The increasing frequency and scale of emergencies requires nutrition to be addressed in all phases of a response.
Humanitarian crises have a negative impact on the health, hygiene, sanitation, and social/care situation for affected populations. Acute malnutrition often increases in the immediate aftermath of an emergency due to the high burden of disease and inadequate diet. Emergencies can also have a negative impact on stunting, infant and young child feeding practices, and micronutrient status of vulnerable groups.
An important component of the U.S. Agency for International Development's (USAID's) Multi-Sectoral Nutrition Strategy is to prevent and manage acute malnutrition in emergencies and in development settings. In emergencies, we aim to prevent increases in stunting or micronutrient deficiencies and to promote optimal infant and young child feeding practices during crises. USAID is committed to the World Health Assembly target which is to "Reduce and maintain childhood wasting to less than 5 percent" and "in humanitarian crises maintain GAM below the emergency threshold of 15 percent." In order to achieve this, clear links between humanitarian response programs and existing development-based nutrition programs should be made at every phase of an emergency response. This brief describes approaches, tools, and products used for nutrition emergency responses and the linkages with nutrition development programs.
Scope of the Problem
More than 52 million children worldwide are suffering from acute malnutrition.2 Of these, approximately 20 million are severely acutely malnourished and, therefore, 9 times more likely to die.3,4 The majority of these children (two-thirds) live in South Asia and Sub-Saharan Africa.5 While acute malnutrition indicates the severity of emergencies in the current situation, chronic malnutrition, or stunting, may also be prevalent in the same populations as these countries are often susceptible to repeated emergencies from which recovery may not be fully realized due to their frequency and the effects of extreme poverty and inadequate resilience in social and economic structures. Every year, approximately 2 million children are treated with life-saving treatment through the Community Management of Acute Malnutrition (CMAM).6 Access to CMAM is increasing as countries scale up these services.
The Impact of Emergencies on Nutritional Status
The two immediate causes of acute malnutrition, disease, and inadequate food intake are common problems during humanitarian crises. Following a natural disaster or in times of conflict, communicable diseases are likely to spread more easily due to a higher concentration of people in one place and displacement. Additionally, poor distribution of health services can result in a lack of access to treatment and consequent disease spread. Diarrhea is particularly common when people are living in an unhygienic setting with inadequate access to sanitation and hygiene materials and facilities. Food supply may be disrupted as markets may not function due to destruction of roads and other infrastructure. Similarly, access to fresh fruits and vegetables and/or animal source protein may be compromised. While food assistance programs aim to provide adequate calories, protein, fat, and micronutrients, young children's specialized needs are difficult to meet.
Infant and young child feeding practices are often negatively affected during emergencies, and this can result in an increase in malnutrition in young children. Babies 6-23 months are the most affected since this is when complementary foods are introduced and children's diets begin to diversify to meet their growth requirements. Emergencies can set back this important milestone if diets are inadequate and available food is unsanitary or unsafe, exposing children to pathogens that cause illness. Mothers may be affected by multiple stresses and unable to breastfeed sufficiently or care for their infants optimally.
Components of Emergency Nutrition Response
Nutrition Information
Integrated Food Security Phase Classification (IPC)
The IPC is a set of analytical tools, and processes, to analyze and classify the severity of a food security situation according to scientific international standards. The IPC standardized scale categorizes the severity of acute food insecurity into Five Phases, based on analyzing a range of outcomes including food consumption levels, livelihoods changes, nutritional status, and mortality. The Five Phases are:
- Minimal
- Stressed
- Crisis
- Emergency
- Famine
Once an emergency has been identified [see box on IPC7], there are three main types of nutrition information used to define and monitor a nutrition crisis.
Survey data: Standardized Monitoring and Assessment of Relief and Transitions (SMART) is the methodology used to conduct household- level surveys to estimate malnutrition prevalence. Basic anthropometry, morbidity and sometimes mortality data are collected during these surveys. If SMART survey data are not available, estimates are also taken from DHS/MICS surveys.
Rapid assessments: Assessments may be conducted by non-governmental organizations or government bodies to quickly gauge the severity of a situation. Assessments are ideally household based and incorporate mid-upper arm circumference (MUAC) screening on a mass scale. The quality of rapid assessments varies widely8, and some countries have national guidelines that outline a methodology. During L2 or L3 emergencies, Interagency Standing Multi-Cluster/Sector Initial Rapid Assessment (MIRA) [PDF, 1.1MB] surveys are conducted to determine humanitarian needs in various sectors. Often, rapid assessments determine that better, more representative data are needed, and a survey is recommended as follow-up.
Program monitoring data: Emergency nutrition response interventions, such as CMAM and IYCF-E described below, have robust performance monitoring systems that collect data on individual children related to recovery, relapse, default, death, attendance, illnesses, etc.9 These data provide insight into the current nutrition situation and also allow a trend analysis over time to understand the factors contributing to malnutrition in the particular emergency situation.
Identification Of Acute Malnutrition
According to the World Health Organization (WHO) Child Growth Standards,10 acute malnutrition is defined as weight-for-height (WFH) z-scores, or MUAC measurement below accepted thresholds for a reference population. Bilateral edema, or kwashiorkor,11 is one of the defining criterions of severe acute malnutrition.
There is no global consensus on whether to use MUAC versus WFH to select children for admission for treatment of acute malnutrition and for discharge when measurements improve. However, MUAC has been demonstrated to be more predictive of mortality (Briend, et al, 1986) and is, therefore, used at the first stage of screening to refer children for additional assessment. Whether using MUAC or WFH, the results select slightly different children: "A low MUAC was more associated with stunting, younger age, being a female, and nutritional edema than a low WHZ."12
Most countries use MUAC for screening and WFH and/or MUAC for admission for treatment and discharge when measurements improve. The ideal increase in MUAC measurement for discharge is still unknown. Many factors must be considered when choosing MUAC or WFH for admission including location, resource availability, etc. The best guidance is to consult national guidelines, the national nutrition sector, or emergency nutrition coordinators.
|
Criterion |
Severe Acute Malnutrition (SAM) |
Moderate Acute Malnutrition (MAM) |
|
Z-score |
≤ -3 Z-score |
>-3 to ≤-2 Z-score |
|
MUAC |
≤ 115 mm |
>115 to ≤ 125 mm |
|
Edema |
Presence of bilateral pitting edema |
|
Management of Acute Malnutrition
The WHO Guidelines for the Management of Acute Malnutrition13 were updated in 2013 where CMAM was endorsed as the best approach to treat uncomplicated acute malnutrition in children between 6 and 59 months in their communities. CMAM increases treatment coverage, improves quality of care and allows for earlier detection and treatment of acute malnutrition (Collins, et al, 2006). Approximately 70 countries have adopted some form of the CMAM approach, but challenges remain. Challenges include staff capacity and supply shortages since specialized therapeutic nutritious foods are critical for this model to be effective (for additional information, please refer to the technical resources listed below as well as the CMAM Technical Brief).
Infants under 6 months require specialized medical care when acutely malnourished. The service delivery model used to address the needs of acutely malnourished infants is called Management of Acute Malnutrition in Infants, (MAMI).14 MAMI supports treatment for infants with lactation support for mothers to improve breastmilk quality and quantity.
Infant and Young Child Feeding in Emergencies (IYCF-E)
IYCF-E [PDF, 920KB]15 includes three main components:
- Promotion of exclusive breastfeeding for 6 months and continued breastfeeding up to 2 years and beyond
- Supporting households to introduce complementary foods at 6 months and continue feeding safe and nutritious foods to children
- Controlling the availability of breastmilk substitutes for the rare situations in which they might be needed
The first component of IYCF-E is promoting exclusive breastfeeding for 6 months and continued breastfeeding. Much of this is done through the social and behavior change communication activities noted below. Success also requires an understanding of women's workload, household support, common cultural practices, religious beliefs, etc.
The second component of IYCF-E response is assuring adequate complementary foods during an emergency, particularly for children between 6 and 23 months, which is when children are most at risk for wasting. Assessing the quality and availability of complementary foods, supporting mothers and caregivers to feed the minimum number of meals per day with the requisite number of food groups is linked to social and behavior change activities noted below.16
The final component of IYCF-E response is the prevention and control of unsolicited donations of breastmilk substitute17 and controlled provision of breastmilk substitute when deemed necessary. Despite the ratification of the International Code of Marketing of Breastmilk Substitutes [PDF, 128KB] by many countries, nearly every emergency provides a new example of inappropriate donations of powdered infant formula and other infant foods. These donations have been shown to displace breastfeeding in crises, and the intervention is generally unsustainable after the supply of free distribution runs out. USAID's ADS 212.3.2 Policy for Breastfeeding Promotion and Protection (revision forthcoming) addresses this important issue. Concerted efforts among emergency workers in nutrition, food security, and logistics are needed in order to prevent, control, and track these donations at all levels. In some emergencies, it is necessary to provide breastmilk substitute for mothers who cannot breastfeed or for infants who have lost their mothers. Some examples include: the earthquake in Haiti, when there were infants who had lost their mothers and were provided with Ready-to-Use Infant Formula; the Syria crisis, where mothers were not breastfeeding pre-war has resulted in some provision of PIF in a controlled manner.
IYCF-E has a large Social and Behavior Change Communication (SBCC) component that is implemented at national, regional, community, household, and individual levels. Some examples of SBBC approaches to address IYCF-E needs include: mother-to-mother support groups, care groups, positive deviance hearth, peer support groups, breastfeeding support groups, baby tents, baby-friendly initiatives/communities, and baby corners. The complementary feeding support activities are aimed at households with food insecurity or where a specialized therapeutic or supplemental food is available for children 6–59 months. There is also a clinical component of individual personal communication and counseling, particularly related to lactation. These activities can be implemented at a health center/post, community, or at the household level.
Standard WHO indicators used to monitor IYCF-E responses include rates of exclusive breastfeeding, continued breastfeeding; the introduction of solid, semi-solid, or soft foods; the minimum meal frequency; the minimum dietary diversity; the minimum acceptable diet; and the consumption of iron-rich foods.
IYCF-E activities are linked to CMAM as part of the overall program to assess and counsel children and their mothers and/or caregivers. IYCF-E can be part of WASH, health, food security, and social protection efforts as well. It should be systematically included as a component of emergency nutrition response.
Integrated Response
An emergency nutrition response is ideally implemented through the existing health system and in collaboration with the Ministry of Health. CMAM and IYCF-E responses are often implemented by community health workers who may receive additional training and supervision from international non-governmental organizations that are experts in emergency responses. Additionally, nutrition should be incorporated into emergency response efforts in other sectors, particularly food security and agriculture, and WASH. Outlined below are ways nutrition and other sectors can be combined to improve nutrition outcomes.
WASH
The WASH and Nutrition brief explains multiple ways to integrate water, sanitation and hygiene (WASH) and nutrition programming and why this programming is so critical. Some programmatic examples of how emergency nutrition response integrates WASH include:
|
Facility Level (CMAM site) |
Community Level |
Household Level |
|
During community screening, active case finders can disseminate messages on the links between malnutrition and poor hygiene (with a focus on handwashing and food hygiene) |
During home visits, active case finders should monitor the following WASH indicators:
|
Food Security and Nutrition
During emergencies, food security is threatened by a disruption of markets, decreased production, loss of assets used to purchase food, etc. Food security programming and nutrition are often occurring in the same communities and households. Food security response in emergencies can include a wide range of interventions ranging from: food assistance, agricultural interventions, livestock interventions and fisheries, income generation activities, and cash-based interventions.19 Agricultural interventions can range from encouraging homestead production, promoting the production of more micronutrient rich foods, improving post-harvest handling, and promoting sustainable agriculture practices. Cash-based interventions can include cash-for-work or cash transfers with the objective to improve household food security. Ideally, any of the above interventions provide an opportunity to include IYCF-E programs, preventing and treating micronutrient deficiencies and providing overall education around diet adequacy.
Nutritional Products
Increased availability of nutritional products to prevent and treat acute malnutrition has greatly improved treatment quality and coverage. But as additional products continue to be available, product choice can be confusing. The following provides an overview of products used to treat and prevent moderate acute malnutrition. Products used for treatment of severe acute malnutrition are covered separately in the CMAM Technical Brief. For information on Ready-to-Use Therapeutic Food (RUTF) and therapeutic milks (F75 and F100), please refer to the forthcoming CMAM Technical Brief and CMAM resources.
Ready-to-Use Foods (RUFs) have many possible uses and many producers. Since many products fall under this category, it is difficult to track the quality and utility. Specific to MAM treatment, most countries have national guidelines which dictate that MAM be treated with either Ready-to-Use Supplementary Food (RUSF) or Fortified Blended Flours (FBF), with the treatment ration defined according to MUAC and/or weight-for-height z-score (WHZ) admission criteria. Other RUFs may be used to prevent acute malnutrition through blanket feeding, where all children of a specified age receive a ration, or used as a discharge ration to prevent relapse of SAM. Some examples include Plumpy'DozTM or a supplementary ration of RUSF. Other RUFs used for development programming or targeted for pregnant and lactating women are outlined in the product chart below and further explained in the Global Nutrition Cluster (GNC) MAM Decision Tool [PDF, 2.0MB].20
Examples from the Field
Integrating Emergency and Development in Ethiopia
- Despite positive economic growth in Ethiopia, more than 225,000 children continue to be affected by SAM each year. The Office of U.S. Foreign Disaster Assistance (OFDA) has been supporting a Rapid Response Mechanism (RRM) to quickly establish CMAM programs in hotspot woredas for the past decade. Much of global guidance on emergency nutrition responses has been developed based on the Ethiopian experience, but the challenge remains to prevent repeated cycles of acute malnutrition emergencies. USAID is supporting programs that merge long-term household livelihood support through the Mission's ENGINE program with OFDA's RRM response through GOAL (a non-governmental organization). Through this model, a small number of woredas in Southern Nations, Nationalities, and Peoples' Region SNNPR receive both ENGINE livelihood support through Save the Children and SAM treatment through the MOH with capacity support from GOAL. The integrated program includes: Integrated provision of Maternal and Infant and Young Child Nutrition into CMAM in 50 percent of GOAL kebeles.
- Capacity support to MOH staff to implement CMAM.
- Provision of chickens, heifers, and training on livestock management to mitigate the routine effects of the hunger season.
Rapid Response Mechanism in South Sudan
In December 2013, conflict in South Sudan forced thousands of families to flee their homes, exhausting already thin coping mechanisms. Women and children were the worst affected, and malnutrition levels increased to unprecedented levels. With two counties having reported Integrated Phase Classification (IPC) Phase 5 "catastrophic," the focus of the emergency response was to focus on life-saving needs of malnourished children. In an effort to reach as many children as possible, FFP and OFDA are implementing a Rapid Response Mechanism through UNICEF and WFP, which has reached more than 154,000 children under-5 with treatment for acute malnutrition, preventive blanket feeding, where all children of a specified age group receive a ration, and general food distribution in inaccessible areas. Staff reach areas by helicopter and screen children under-5 using MUAC tapes. Malnourished children receive a ration of RUTF, and all children receive a preventive de-worming and vitamin A supplementation.
IYCF in Emergencies – an Example from Haiti
Following the devastating earthquake in Haiti in 2010, OFDA supported the establishment of 193 baby tents throughout Port au Prince, Leogane and Jacmel to provide a safe place for mothers to breastfeed and for caregivers of infants who had lost their mothers to receive Ready-to-Use Infant Formula (RUIF) following a detailed assessment.21 More than180,499 mother-baby pairs received lactation and psychosocial support in the 12 months following the earthquake. OFDA provided containers of RUIF which were used as a breastmilk substitute for one year following the earthquake. This prevented newborns from being exposed to dangerous pathogens as a result of PIF preparation, or inadequate nutritional content from inferior BMS or local preparations. Moreover, the importance of IYCF was highlighted in all of Haiti and the Ministry of Health, in collaboration with the nutrition staff, developed guidelines for the baby tents, as well as a revised IYCF strategy for national roll-out.
Technical Resources
CMAM
www.unicef.org/media/files/Community_Based__Management_of_Severe_Acute_Malnutrition.pdf [PDF, 948KB] ]
Global Nutrition Cluster MAM Decision Tool
nutritioncluster.net/wp-content/uploads/sites/4/2014/07/MAM-Decision-Tool-final-June-2014-corrected.pdf [PDF, 2.0MB]
SMART methodology
smartmethodology.org/
IFE Operational Guidance
www.ennonline.net/operationalguidanceiycfv2.1
Save the Children IYCF-E toolkit
sites.google.com/site/stcehn/documents/iycf-e-toolkit
Optifood
www.fantaproject.org/tools/optifood
This Technical Brief will be periodically updated. Comments from readers are welcome to Leslie Koo, especially comments to help clarify the information provided or where additional information may be useful. (Last updated February 7, 2016.)
References
Collins, S., et. al. 2006. Management of Severe Acute Malnutrition in Children. Lancet 368 (9551):1992-2000.
Briend, A., Zimicki, S. Validation of Arm Circumference as an Indicator of risk of death in one to four year old children. Nutr Res. 1986;6:249–61.
Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community-based therapeutic care programs. Food Nutr Bull. 2006;27:s7–23.
Puett C, Coates J, Alderman H, Sadler K. Quality of care for severe acute malnutrition delivered by community health workers in southern Bangladesh. Matern Child Nutr. 2013;9:130–42.
Roberfroid et al, 2013, Utilization of mid-upper arm circumference versus weight-for-height in nutritional rehabilitation programmes: a systematic review of evidence, WHO.
Sadler, K. Puett, C. Mothabbir, G. & Myatt, M. 2011. Community Case Management of Severe Acute Malnutrition in Southern Bangladesh.
Talley L, Boyd E, el Sharief F, Blanton C, OmerAli M, et al. (2012) Prevention of Acute Malnutrition During the Lean Season: Comparison of a Lipid-Based Nutrient Supplement and an Improved Dry Ration, South Darfur, Sudan. A quasi-Experimental Study. J Nutr Disorders Ther 2:117.
Walter T, Sibson V, McGrath M. Mid Upper Arm Circumference and Weightfor- Height Z-score as Indicators of Severe Acute Malnutrition. 2012
A Joint Statement by the World Health Organization, the World Food Programme, the United Nations Standing Committee on Nutrition and the United Nations Children's Fund. Community based management of severe acute malnutrition. Geneva: World Health Organisation; 2007.
Endnotes
1. OCHA (2015).
2. World Bank 2015, Joint Child Nutrition Estimates (UNICEF/ WHO/ World Bank)
3. United Nations Children's Fund, World Health Organization, & The World Bank (2012). Levels and trends in child malnutrition. Joint child malnutrition estimates. New York, NY: United Nations International Children's Fund; Geneva:World Health Organization;Washington, DC:World Bank.
4. Black et al. 2008 Need full citation.
6. UNICEF, 2013, Global SAM Management Update
7. Integrated Food Security Phase Classification
8. Rapd Assessment Method: Development Update: Number 2 [PDF, 194KB]
9. CMAM Report
10. The WHO Child Growth Standards
11.UNICEF definition: Nutritional edema (or kwashiorkor) is characterized by bilateral pitting edema (affecting both sides of the body) in the lower legs and feet which as it progresses becomes more generalized to the arms, hands and face.
12. Roberfroid et al, 2013, Utilization of mid-upper arm circumference versus weight-for-height in nutritional rehabilitation programmes: a systematic review of evidence, WHO.
13. WHO, 2013, Management of Severe Acute Malnutrition
14. www.who.int/elena/titles/full_recommendations/sam_management/en/
15. Infant and Young Child Feeding in Emergencies [PDF, 920KB]
17. Operational Guidance on Infant and Young Child Feeding in Emergencies v 2.1 (2007)
18. Particularly at critical times: after cleaning a baby following urination/defecation; before preparing food (especially complementary foods); before and after active feeding of a child.
19. ACF International, 2012, Maximising the Nutritional Impact of Food Security and Livelihood Interventions [PDF, 2.6MB]
20. GNC, MAM Decision-Tool, revised
21. Ayoya et al. (2012), Protecting and improving breastfeeding practices during a major emergency: lessons learnt from the baby tents in Haiti [PDF, 1.0MB], Bull World Health Organ 2013;91:612–617.

Comment
Make a general inquiry or suggest an improvement.