- What We Do
- Agriculture and Food Security
- Democracy, Human Rights and Governance
- Economic Growth and Trade
- Education
- Environment and Global Climate Change
- Gender Equality and Women's Empowerment
- Global Health
- Humanitarian Assistance
- Transformation at USAID
- Water and Sanitation
- Working in Crises and Conflict
- U.S. Global Development Lab
Speeches Shim

At a Glance
- Multi-Sectoral Nutrition Strategy
- History of CMAM
- Components of CMAM
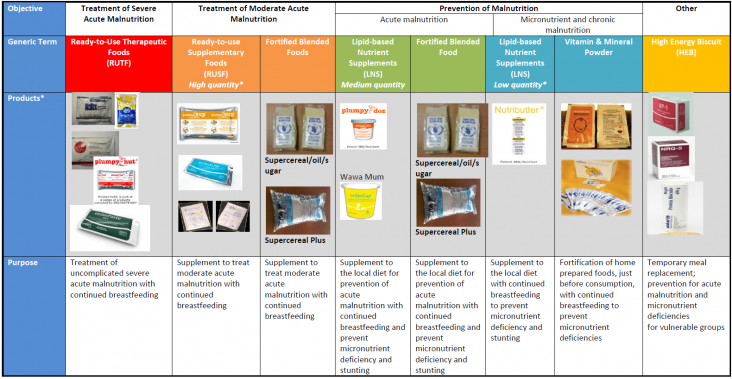
- Nutrition Products Used int he Management of Acute Malnutrition
- Considerations for Supporting CMAM
- References
- Websites, Tools and Guidance Documents
- Endnotes
View the PDF [PDF, 925KB].
In 2016, 156 million children under-5 suffered from stunting. The consequences are dire: a child with severe acute malnutrition (SAM) is 11.6 times more likely to die, and a child with moderate acute malnutrition (MAM) is 3 times more likely to die than a well-nourished child (Olofin, 2013).1 Acute malnutrition is characterized by rapid weight loss and/or nutritional edema2 caused by illness and/or inadequate food intake, such as a sudden change in the quality and/or quantity of food or poor infant feeding practices. It often increases during humanitarian crises but occurs during non-emergency situations as well.
Among children under-5 worldwide, 50 million children suffered from wasting in 2016. The Lancet series identified 10 high-impact, nutrition-specific interventions that, if taken as a package to 90 percent coverage, could reduce wasting by 60 percent and stunting3 by 20 percent (Bhutta, 2015). The management of SAM and MAM are 2 of the 10 interventions. Community Management of Acute Malnutrition (CMAM) is a proven approach to manage SAM and MAM in children under 5 and is currently implemented in more than 70 countries (UNICEF, 2013).
Definitions of SAM and MAM
Acute malnutrition is measured by:
- low weight-for-height index, also called wasting
- low mid-upper arm circumference (MUAC)
- nutritional edema
Severe acute malnutrition is defined by a weight-for-height index <-3 z-score, MUAC <11.5 cm, and/or nutritional edema.
Moderate acute malnutrition is defined by a weight-for-height index <-2 and ≥-3 z-score, and/or MUAC <12.5 and ≥11.5 cm.
CMAM classifies SAM in children as complicated or uncomplicated. Complicated SAM cases, which represent approximately 10–20 percent of all children with SAM, refer to children without an appetite and/or with medical complications such as a high fever, severe dehydration, and lower respiratory infection. The children are stabilized in 24-hour inpatient care facilities before referral to continue treatment at decentralized outpatient care facilities. Uncomplicated SAM cases refer to children with no medical complications and with an appetite. These children are managed at home with weekly or biweekly visits at a nearby health facility. All children receive essential medical care as part of the management of malnutrition. Community-based mobilization, screening, follow-up, counseling, and education are a cornerstone of CMAM, allowing for earlier detection of malnutrition, continuous monitoring of care, and linkages with other services. By offering case management at decentralized sites and incorporating community activities, the approach increases coverage, access, and effectiveness of treatment for acute malnutrition.
USAID Multi-Sectoral Nutrition Strategy
Recognizing the importance of CMAM to achieving its targets, the U.S. Agency for International Development (USAID) Multi-Sectoral Nutrition Strategy endorses the scale-up and strengthening of the CMAM approach in areas where USAID works (USAID, 2014). The strategy promotes establishing linkages with complementary programs, strengthening professional and institutional capacity to implement CMAM services, and supporting the enabling policy environment as well as direct service delivery. The CMAM approach is also the launching point for scaling up access to treatment of malnutrition during humanitarian emergencies – building surge capacity among the health staff and pre-positioning of nutrition products (see the USAID Nutrition in Emergencies Brief for additional discussion).
History of CMAM
Client Flow in a Comprehensive CMAM Approach
A comprehensive CMAM approach will vary by context, but the client flow will likely involve these steps:
- Community-based health workers screen children for acute malnutrition using mid-upper arm circumference tapes and refer those identified with SAM or MAM to the nearest health center.
- If a child is identified as acutely malnourished, the caretaker takes the child to the health center where the health worker conducts further screening and diagnosis according to the established protocol. The health worker takes anthropometric measurements and checks for nutritional edema, appetite, and other medical complications. At the health center, the staff also screens other children that have come for pediatric visits.
- If the child has SAM and medical complications or no appetite, the child is admitted to inpatient treatment using therapeutic milks until the complications have stabilized and the child can be transitioned to outpatient care.
- If the child has SAM, no medical complications, and an appetite, the child is treated on an outpatient basis with RUTF.
- If the child has MAM, the child might receive a specialized food product, such as ready-to-use supplementary food (RUSF) or fortified blended food (FBF).
- Once home, the child receives visits from the community-based health worker to check on his/her status and receive counseling, education, and possibly referrals to complementary programs. The child stays in the program until he/she reaches exit criteria, though defaulting (not completing the full course of treatment) is a challenge that most programs face.
Prior to CMAM, children with SAM were treated in inpatient facilities with therapeutic milks, commercially called F75 and F100 (see section on nutrition products). The inpatient model posed many challenges to effective treatment for both health systems and patients – long recovery periods (up to 6 weeks); overcrowding and cross-infection; high opportunity costs for families to access and remain in treatment; costly and resource-intensive services for health systems to sustain; concerns about safe preparation and storage of therapeutic milks; and low coverage of services. In the mid-1990s, ready-to-use therapeutic food (RUTF) was developed as an alternative to therapeutic milk (F100) that could be safely consumed at home. This innovative product allowed treatment for uncomplicated cases of SAM to be shifted to the home, paving the way for CMAM. The first pilot project tested the CMAM approach in 2000 during humanitarian emergencies (Collins, 2002). It was found to be so effective that it was endorsed by United Nations (U.N.) agencies in 2007 (WHO et al., 2007) and is now considered the standard of care for managing acute malnutrition in emergency and development contexts.
Components of CMAM
The CMAM approach is comprised of four components: (1) community outreach and mobilization; (2) outpatient management of SAM without medical complications; (3) inpatient management of SAM with medical complications; and (4) services or programs to manage moderate acute malnutrition (MAM), such a supplementary feeding program (see textbox on the client flow in a comprehensive CMAM approach). Implementation of the various components of CMAM can vary across geographic areas and implementers, but all CMAM programs include the outpatient management of SAM without medical complications and are designed with a community component. Some national protocols have special consideration for people living with HIV and/or tuberculosis (TB), and include older age groups (e.g., in Mozambique).
Some CMAM programs include MAM management, while others do not. This is partly a reflection of the absence of normative global guidance for MAM management, compared to SAM management for which normative guidance is readily available.4 Resources may also be more constrained for managing MAM, which has a lower risk of death compared to SAM and, therefore, may be deemed a lower priority. Given the high global burden of MAM (an estimated 33 million children) (UNICEF et al., 2012) and the fact that the prevention and treatment of MAM reduce the incidence and severity of SAM, it is important for CMAM programs to consider incorporating MAM management and prevention either as part of the CMAM program itself or through links with complementary programs.
The management of acute malnutrition in infants under 6 months, a highly vulnerable group with an increased risk of mortality, is generally included in national protocols, though stronger evidence-based guidance is needed. The current focus is on inpatient treatment for infants while supporting breastfeeding; infants under 6 months with acute malnutrition do not receive RUTF.
Nutrition Products Used in the Management of Acute Malnutrition
National treatment protocols for the management of acute malnutrition include essential medical treatment such as antibiotics, vitamin A supplements, malaria prophylaxis, deworming treatment, measles vaccination, and iron or folic acid supplements, as well as the following specialized nutrition products:
- RUTF is a lipid-based, energy-dense, mineral‐ and vitamin‐enriched food specifically designed to treat SAM in children 6 to 59 months. RUTF has a similar nutrient composition to F100, does not require cooking, and is safe for in-home consumption.
- RUSF has similar properties to RUTF, but one of its formulations is specifically designed to treat MAM in children 6 to 59 months.
- FBF are blends of partially precooked and milled cereals, soya, beans, and pulses fortified with vitamins and minerals, and may contain vegetable oil or milk powder.
- F75 and F100 are therapeutic milks used in inpatient treatment of SAM. They provide 75 and 100 kilocalories for every 100 milliliters, respectively.
- Rehydration solution for malnutrition (ReSoMal) is oral rehydration solution specifically for severely malnourished children.
- Combined Mineral and Vitamin Mix is used to make F75 and F100 therapeutic milks from local ingredients (milk, oil, and sugar), and ReSoMal from the commonly-available oral rehydration solution.
RUTF, RUSF, and FBF are further described in the below product table, along with specialized nutrition products for the prevention of malnutrition and for temporary meal replacements (Global Nutrition Cluster, 2014).
Considerations for Supporting CMAM
CMAM integration into the national health systems. In nearly all countries, CMAM services are delivered as part of regular health services or as a combination of regular and emergency services. Although most ministries of health assume leadership and coordination roles and have established partnerships with U.N. agencies, World Health Organization (WHO), donors, and non-governmental organizations, not all elements of CMAM service delivery are fully integrated into national health systems (UNICEF, 2013). Health system capacity and the cost of specialized nutrition products are major challenges with full integration into national health systems. Some countries have made notable strides in integrating the management of SAM into health services delivery including Ethiopia, Malawi, and Niger (Deconinck et al., 2011). WHO and the United Nations Children's Fund (UNICEF) are leading an interagency task force to develop guidance on the integration and scale-up of the management of SAM. Resources on integrating CMAM into national health systems are also available through publications5 and reports of major workshops (Emergency Nutrition Network, et al., 2008).
Elements of quality programming.The quality and effectiveness of CMAM services depends on a number of factors. On the health systems side, there needs to be an enabling policy environment; sustained financing; a competent and responsive workforce; consistent stock of equipment; timely availability of supplies; supportive environment in which quality services are delivered; and information management systems to monitor implementation and make course correction where needed. Additionally, the community component should be strong enough to mobilize, screen, refer, and follow up cases, in addition to providing nutrition education and counseling and other activities aimed at managing and preventing malnutrition. To utilize services, people need to have physical access to the health centers, be motivated enough to go to the first visit, continue to go to subsequent visits, and follow the regimen at home until the person has been discharged and, ideally, referred to complementary programs such as those that address the conditions that led to malnutrition. Programming should also be sensitive to gender, ensuring that roles and responsibilities for managing and preventing malnutrition are encouraged equally for men and women. The resources listed at the end of this brief provide guidance and tools to plan for and strengthen quality programming.
Linkages with complementary services and programs. Linking CMAM with complementary services and programs – such as those promoting maternal, infant, and young child nutrition; micronutrient supplementation; water, sanitation, and hygiene (WASH); HIV care and treatment; early childhood development (ECD); and livelihoods, agriculture, and food security – has the potential to expand coverage and effectiveness. Children attending growth monitoring and promotion services, for example, may be screened and referred for acute malnutrition. CMAM personnel may be trained to support recommended infant and young child feeding (IYCF) practices with caregivers at key contact points; and IYCF counselors may be trained to screen, refer, and follow up children with acute malnutrition. Caretakers of malnourished children may be referred to social safety net programs aimed at improving the household's livelihood and food security status (see also the Nutrition in Emergencies Brief, the WASH and Nutrition Brief, and the Nutrition and ECD Brief for additional discussion). In Kenya, the government introduced a package of 11 high-impact nutrition interventions focusing on CMAM, infant feeding, food fortification, and micronutrient supplementation at the health facility and community levels. An initial evaluation showed many positive outcomes, including that ownership by the district health teams increased, coordination improved, and the number of clients receiving the services, including for CMAM, increased (UNICEF, 2012).
In some countries where the nutrition assessment, counseling, and support (NACS) approach has been implemented as a set of programmatic interventions, CMAM and NACS are integrated (e.g., in Mozambique and Namibia); are in the process of being combined (e.g., in Malawi); or are run in parallel, where the NACS program treats acute malnutrition in people living with HIV and/or TB, while the CMAM program treats cases of acute malnutrition in children under 5 (Castleman and Diene, 2015). In places where CMAM and NACS coexist, it is important to harmonize and coordinate standards and protocols to the extent possible to ensure a consistent quality of care across demographic groups.
Additionally, programs aimed at the management of acute malnutrition and/or the prevention of chronic malnutrition should also consider the degree to which integration or linkages may be made, taking into consideration contextual factors. Historically, acute, and chronic malnutrition have been treated as separate rather than related conditions, with acute malnutrition programs focused on medicalized treatment and chronic malnutrition programs focused on longer-term preventive approaches (Bergeron and Castleman, 2012). However, wasting and stunting have common risk factors, and evidence suggests that wasting adversely affects linear growth, and wasting recovery benefits linear growth (Khara and Dolan, 2014).
Though there is a paucity of evidence and operational guidance on making effective linkages, some programmatic guidance and examples exist.6 UNICEF recommends that inter-sectoral links initially be tested and documented on a small scale to assess whether they do, in fact, benefit each other and result in more efficient use of resources (UNICEF, 2015).
References
Bergeron, Gilles and Castleman, Tony. 2012. "Program Responses to Acute and Chronic Malnutrition: Divergences and Convergences." Advances in Nutrition. Volume 3, pp. 242-249.
Bhutta, Zulfiqar A, et. al. 2013. "Evidence-Based Interventions for Improvement of Maternal and Child Nutrition: What Can Be Done and At What Cost?" The Lancet. Volume 382, Issue 9890, pp. 452-477.
Castleman, Tony and Diene, Serigne. 2015. Technical Brief: The Role of Nutrition Assessment, Counseling, and Support in Health Systems. Washington, DC: FHI 360/FANTA.
Collins, Steve and Sadler, Kate. 2002. "Outpatient Care for Severely Malnourished Children in Emergency Relief Programmes: A Retrospective Cohort Study." The Lancet. Volume 360, Issue 9348, pp. 1824-1830.
Deconinck, Hedwig, et al. 2011. Review of Community-Based Management of Acute Malnutrition Implementation in West Africa: Summary Report. Washington, DC: FHI 360/FANTA-2 Bridge.
Emergency Nutrition Network and FANTA. 2008. International Workshop on the Integration of Community-Based Management of Acute Malnutrition: Workshop Report. Washington, DC.
Global Nutrition Task Force, MAM Task Force. 2014. Moderate Acute Malnutrition: A Decision Tool for Emergencies [PDF, 2.0MB] .
Khara, Tanya and Dolan, Carmel. 2014. Technical Briefing Paper: Associations between Wasting and Stunting, Policy, Programming, and Research Implications. Emergency Nutrition Network.
Olofin, Ibironke, et al. 2013. "Associations of Suboptimal Growth with All-Cause and Cause-Specific Mortality in Children under Five Years: A Pooled Analysis of Ten Prospective Studies." PLOS One. 8(5): e64636.
UNICEF, WHO, and The World Bank. 2012. UNICEF-World Bank Joint Child Malnutrition Estimates [PDF, 7.1MB]. New York: UNICEF; Geneva: WHO; Washington, DC: The World Bank.
UNICEF. 2012. Evaluation of Integrated Management of Acute Malnutrition (IMAM): Kenya Country Case Study. New York: UNICEF.
UNICEF. 2013. Global Evaluation of Community Management of Acute Malnutrition (CMAM): Global Synthesis Report. New York: UNICEF.
UNICEF. 2014. Nutridash 2013: Global Report on the Pilot Year [PDF, 5.7MB]. New York: UNICEF.
UNICEF. 2015. Management of Severe Acute Malnutrition in Children: Working Towards Results at Scale. New York: UNICEF.
USAID. 2014. Multi-Sectoral Nutrition Strategy 2014–2025. Washington, DC: United States Agency for International Development.
WHO, World Food Programme, U.N. System Standing Committee on Nutrition, and UNICEF. 2007. Community-Based Management of Severe Acute Malnutrition: A Joint Statement by the WHO, World Food Programme, U.N. System Standing Committee on Nutrition and UNICEF. New York: UNICEF.
Websites, Tools and Guidance Documents
- The Coverage Monitoring Network
- The CMAM Forum
- The Emergency Nutrition Network
- The Food and Nutrition Technical Assistance III Project
- USAID Global Nutrition
- Valid International website
- The CMAM Costing Tool
- The UNICEF Nutrition Dashboard (NutriDash) [PDF, 5.7MB]
- The CMAM Report
- UNICEF Program Guidance on Management of SAM[PDF, 1.2MB]
- USAID webpage on USAID RUTF
- WHO Guidance on SAM management:
- WHO (1999). Management of severe malnutrition: a manual for physicians and other senior health workers. Geneva: WHO; 1999.
- WHO (2003). Guidelines for the Inpatient Treatment of Severely Malnourished Children [PDF, 391KB].
- WHO (2013). Guideline: updates on the management of severe acute malnutrition in infants and children [PDF, 2.1MB].
This Technical Brief will be periodically updated. Comments from readers are welcome to Leslie Koo, especially comments to help clarify the information provided or where additional information may be useful. (Last updated January 28, 2016)
Endnotes
1 "Well-nourished" in this reference refers to weight-for-height ≥ -1 z-score.
2 Nutritional edema is also referred to as bilateral pitting edema. It is the excessive accumulation of fluid in body tissues resulting from severe nutritional deficiencies.
3 Stunting is measured by height- or length-for-age <-2 z-score and is an indicator of chronic malnutrition.
4 See guidance documents for SAM management listed under "References" in this brief.
5 See Governance page of the CMAM Forum.
6 See for example: UNICEF, 2015 and the "prevention" webpage of the CMAM Forum.

Comment
Make a general inquiry or suggest an improvement.